Clinical Trial Design
Episode Notes
Types of Trials
Screening trials
Designed to improve the discovery of early, asymptomatic disease
Should both identify individuals and prescribe treatment
Prevention Trials
Designed to reduce the effects of a disease
Primary prevention
Investigate ways to reduce the risk of disease occurring
I.e. vaccine trials
Secondary prevention
Designed to identify treatment of early-stage disease, thereby reducing risk of progression to later stage disease
Tertiary prevention
Designed to identify interventions that decrease the morbidity and/or mortality associated with a disease after people have been diagnosed
This is the majority of oncology trials
Phases of Drug Development
Preclinical
Studying the drug in a basic science lab - tumor cell lines, tissue cultures, animals
Phase I
“Safety phase”
Aimed to identify dosages of drugs - specifically, maximum tolerated dose (MTD)
Goal is to identify recommended dose level (RDL) OR recommended phase II dose (RP2D) OR no recommended dose if none of the effective doses are tolerable
Enroll small groups of patients who are administered increasing doses of the developing drug
Clinical responses also recorded but not primary aim
Phase IB Expansion
Take a specific dose or specific subgroup from the initial portion of the phase I trail, then expand its use in that group
Often randomized to two different doses
If no difference in efficacy, then FDA will require the lower dose for next phases
Phase II
“Efficacy Phase”
Investigates whether an agent produces a sufficiently robust response to move to phase 3
How to measure efficacy?
RECIST criteria
Time to first progression or recurrence
Smaller than phase 3 trials and typically not placebo-controlled
Primary outcome usually overall response rate (not PFS or OS)
Phase IIa
Compare response rates to comparative historical control
Multi-arm compares multiple experimental regimens against SOC response rate for that disease site/stage/setting
Phase IIb
Compare response rates of experimental drug to response in patients given SOC in real time
Commonly used for biomarker-specific/targeted therapy trials (often there isn’t an accepted historical response rate)
Safety Lead-In
Small cohort
Allows for quicker movement from phase I to phase II
Can be used for new drug combinations sometimes when toxicities are not anticipated to be that severe
If not severe, then can expand to phase II trial
Example is chemo + IO combination trials
Phase III
Designed to determine efficacy compared to SOC in a specific patient population
Aim is to change SOC and to get FDA approval
Types of Phase III
Superiority: is the intervention better than the SOC?
Accounts for majority
Non-inferiority: is the intervention not worse than the SOC?
Designed to demonstrate that there is something better (i.e. side effects, QOL, cost) with non-inferior oncologic outcomes (i.e. PFS, OS)
Equivalency: rarely used in oncology
“Best”: randomized, blinded, placebo-controlled
Randomization
Assigning participants randomly to the control arm vs experimental arm
Reduces selection bias
Examples: stratified randomly permutated blocks, dynamic treatment allocation
Blinding
Non-disclosure of control vs experimental arm
Single - just the patient
Double - patient and administering physician
Triple - patient, physician, statistician
Placebo
Another way to reduce bias and strengthen integrity of trial
Adaptive Trials
Allows quicker movement from Phase II to Phase III
Allow trial design to change during the trial, based on interim data
Saves resources, allow the trial to progress quicker w/o having to design, accrue, and get approval for two separate trials
Phase IV
Conducted after regulatory approval to evaluate long-term effectiveness, rare adverse events, and real-world outcomes
Clinical Trial Outcomes/Endpoints
Typical Primary Endpoints
Phase I/II: Overall Response Rate
Phase III+: Progression free survival (PFS), overall survival (OS), or progression free survival 2 (PFS2)
Definitions
PFS2: time from randomization (or start of initial therapy) to progression on the next line of therapy or death, whichever occurs first
captures both: duration of disease control on the initial (first-line) treatment (PFS1), AND duration of control on the subsequent therapy after progression
Time to progression (TTP) does not include deaths
Progression free survival (PFS) does include deaths; includes stable disease
Duration of response (DOR): only includes patients with an objective response to therapy
PFS Controversies
Used to be viewed as a good surrogate for OS; not always true now with multiple lines of therapy
Conversely, forcing wait for OS may delay approval
Possible biases:
Assessment of progression bias: due to potential treatment effects, true blinding may not be possible
Blinded Independent Central Review (BICR) of imaging can help overcome this bias
Assessment-time bias: the time point at which you discover a progression is when you will say progression occurs
Assessments in both SOC and experimental arms must be the same
Toxicities/Adverse Events
Standardly graded 1-5
Grade 1: mild; Grade 5: death
Grade 3+ considered “significant”
Treatments adjusted or discontinued at this level
Should compare AE rate of investigational drug to SOC therapy
Patient Reported Outcomes (PROs) / Patient Reported Outcome Measures (PROMs)
PROs are measured by PROMs - validated questionnaires
Help identify and characterize symptoms and toxicities, in addition to measurement of graded adverse events
Best practices
Be efficient and thoughtful about which PROMs you use - pts can experience respondent fatigue and clinical work flow can be burdened by over-collecting
Complement of PROMs should include a general QOL tool and a disease-specific PROM
General QOL PROMs
FACT-G (27 questions) and EORTC QLQ C30 (30 questions) best studied and most commonly used
Can add disease-specific scales - usually increases to ~60 questions
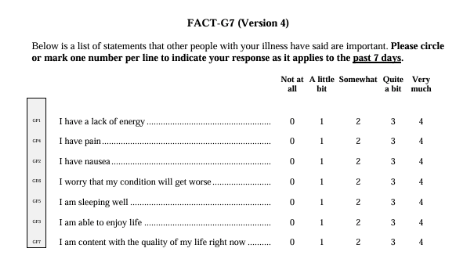
FACT-G7 (7 questions) over 3 domains - physical, emotional, functional well-being
Good for clinical use outside of trials
See Figure 1 for example
FACT-GP5: “I am bothered by the side effects of treatment”
SGO recommends the FACT-G7 + GP5 for use in routine clinical settings
Disease Sites
Ovarian Cancer PROMs
Disease-specific subscales from FACT or EORTC
NCCN/FACT Ovarian Symptom Index (NFOSI): 18-item measure
Uterine Cancer PROMs
FACT-G/FACT-EN (15 items)
EORTC-EN24 (24 items)
SGO states uterine disease is understudied in terms of PROs
Cervical Cancer PROMs
Heterogeneous group when comes to impact on QOL
Anxiety and sexual function concerns very relevant for this group even w/o disease recurrence
FACT and EORTC with cervical cancer add-ins
Vulvar/Vaginal Cancer
Stigma around these diseases so symptoms may not be spontaneously reported by patients
FACT-V (15-items) to add to general QOL PROM
EORTC is developing their scale
Additional Scales
Sexual Function
Up to 80% of female cancer pts report distressing sexual, vaginal, and/or menopausal concerns related to cancer and treatment; 90% say their oncologists don’t ask them about these things!
Female Sexual Function Index (FSFI) - 19 items
Modifiable for sexually diverse population and those who aren’t currently sexually active
PROMISE sexual function and satisfaction measures version 2.0 (PROMIS SexFS v2.0)
Appropriate for patients who are sexually active with or without a partner
EORTC - currently validating a 22 item QLQ-SHQ22
SGO recommended directly asking “would you like to discuss your sexual health?”
Biomarkers
Can be used as outcomes (biomarker change) or as inclusion/selection criteria for clinical trials
Predictive vs Prognostic Biomarkers
Prognostic: refers to the cancer outcome, independent of the therapy received
Predictive: whether the presence of a specific biomarkers impacts the chance of response to therapy
Quantitative Effect: both groups response to therapy but some get a better impact
Qualitative Effect: response vs no response
Proving biomarker is predictive can be challenging - need at least two comparison groups available, need to perform a statistical test for an interaction, and the test for interaction needs to be statistically significant
Clinical Trial Designs
Definitions
Integral biomarker: biomarker-defined criteria for enrollment into a trial
Integrated biomarker: used to test the hypothesis during the study, but isn’t a requirement for enrollment
Biomarker enrichment trials: only include patients with the biomarker expressed
Can reduce required sample size while maintaining power
Helpful if biomarker positivity prevalence is low
Randomized umbrella trials: target one disease of interest, with several different biomarkers being evaluated
Usually hierarchical/prioritized - one biomarker is the “prioritized” biomarker, and if a patient has that one, they’re triaged to that arm; if no, then check next biomarker
Example in endometrial cancer - RAINBO trial - for the different molecular subtypes of endometrial cancer
Basket trials: disease agnostic, test a specific targeted therapy on people w/ many types of tumors, as long as they have a specific biomarker
Example: DESTINY-PanTumor02
Clinical Trial Eligibility
Exists primarily to reduce the influence of confounding variables
Aims to identify the target population and make them similar at baseline
Aims to exclude people in whom toxicities are expected to outweigh benefits
Aims to follow regulatory guidelines regarding eligible populations
Aims to protect personal privacy
Aims to exclude patients who would not be able to comply with the planned intervention
Real-world Issues
Creating “ideal” populations can reduce the generalizability
Historically contributed to preferential enrollment of white patients from high SES who have less comorbidities or other reasons for exclusion
Comorbidity criteria
Tracking the relationship between accrual and comorbid conditions in clinical TRial enrollment (TRACE), Oluloro et al 2024
Aimed to characterize the comorbidity profile of patients with uterine cancer by race and compare w/ expected clinical trial enrollment patterns based on standard/historic Comorbidity Exclusion Criteria (CEC)
>284,000 patients included - 73% white, 14% black, 3% asisan
Odds of clinical trial exclusion based on comorbidities were 2x higher for black vs white patients w/ OR 2.09
Language
Often an exclusion criteria for enrollment
Even when not, still lower rates of enrollment for patients with limited English proficiency
Jorge et al. 2023
Enrollment rate 7.5% for English-speaking vs 2.2% for limited English proficiency
Best Practices for Discussing Clinical Trial Enrollment w/ Patients
Consider enrollments for all patients
Documented belief amongst medical providers that patients of color do not want to participate in research studies
Langfor et al. 2013 (Cancer)
No difference along racial or ethnic lines in clinical trial refusal rates or “no desire to participate in research” as a reason to refuse clinical trial
Common reasons pts decline enrollment
Discomfort w/ randomization and possibly receiving placebo
Fear of experimentation
Concerns about privacy
Time cost of the consent and monitoring process
Highlight values
Clinical benefit for them
Improving our knowledge of how to treat patients in the future
Increased knowledge about their own cancer/genetics
Core Principles
Trials should be offered to all eligible patients without preconceived assumptions about who might or might not be interested in participation
Clinicians should be forthcoming about both the limitations of their knowledge and the hopes informed by earlier phases of investigation
Transparency throughout the process is essential; while the ultimate outcomes of a trial cannot be predicted, patients should be provided with a clear framework of what to expect along the way
Figure 1.
FACT-G7 (7 questions) over 3 domains - physical, emotional, functional well-being; QOL survey
Reference List
1. Sisodia RC, Dewdney SB, Fader AN, et al. Patient reported outcomes measures in gynecologic oncology: A primer for clinical use, part I. Gynecol Oncol 2020;158(1):194–200; doi: 10.1016/j.ygyno.2020.04.696.
2. Sisodia RC, Dewdney SB, Fader AN, et al. Patient reported outcomes measures in gynecologic oncology: A primer for clinical use, Part II. Gynecol Oncol 2020;158(1):201–207; doi: 10.1016/j.ygyno.2020.03.022.
3. Anonymous. Vulva Cancer | EORTC – Quality of Life. n.d. Available from: https://qol.eortc.org/questionnaire/qlq-vu34/ [Last accessed: 4/27/2025].
4. Anonymous. Patient-Reported Outcomes Measurement Information System (PROMIS) | NIH Common Fund. n.d. Available from: https://commonfund.nih.gov/patient-reported-outcomes-measurement-information-system-promis [Last accessed: 4/27/2025].
5. Ballman K V. Biomarker: Predictive or prognostic? Journal of Clinical Oncology 2015;33(33):3968–3971; doi: 10.1200/JCO.2015.63.3651.
6. Oluloro A, Pike M, Moore A, et al. Tracking the relationship between accrual and comorbid conditions in clinical TRrial enrollment (TRACE). Gynecol Oncol 2024;190:S72; doi: 10.1016/J.YGYNO.2024.07.106.
7. Oluloro A, Temkin SM, Jackson J, et al. What’s in it for me?: A value assessment of gynecologic cancer clinical trials for Black women. Gynecol Oncol 2023;172:29–35; doi: 10.1016/j.ygyno.2023.03.002.
8. Jorge S, Masshoor S, Gray HJ, et al. Participation of Patients with Limited English Proficiency in Gynecologic Oncology Clinical Trials. JNCCN Journal of the National Comprehensive Cancer Network 2023;21(1):27–32; doi: 10.6004/jnccn.2022.7068.
9. Montes de Oca MK, Howell EP, Spinosa D, et al. Diversity and transparency in gynecologic oncology clinical trials. Cancer Causes and Control 2023;34(2):133–140; doi: 10.1007/S10552-022-01646-Y/METRICS.
10. Langford AT, Resnicow K, Dimond EP, et al. Racial/ethnic differences in clinical trial enrollment, refusal rates, ineligibility, and reasons for decline among patients at sites in the National Cancer Institute’s Community Cancer Centers Program. Cancer 2014;120(6):877–884; doi: 10.1002/cncr.28483.